In the Obesity Clinic, Obesity Center, Antalya, Turkey, we treat overweight & obesity
The fight against obesity is led by many sufferers for years, accompanied by yo-yo effects or diabetes, back and joint damage, cardiovascular diseases and depression.
Obesity is a chronic disease. For a lasting success of therapy, sufferers have to work for a lifetime. We will not leave you alone.
Bariatric surgery Antalya, Turkey, price, cost,
Gastric Sleeve, Antalya, Turkey, Obesity Center
Bariatric Reduction, Antalya, Turkey, Obesity clinic
Sleeve Gastrectomy Antalya, Turkey, Obesity Center
Gastric Sleeve Resection Antalya, Turkey, Obesity clinic
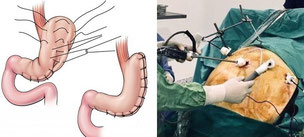
The Stomach surgery, Gastric Sleeve, Stomach Reduction, Sleeve Gastrectomy, Gastric Sleeve Resection, tube magenop, is performed by the English speaking doctor, laparoscopically in Antalya.
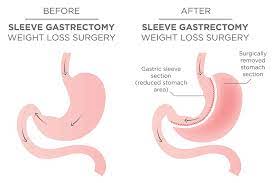
A large part of the stomach is removed, so that only one tube remains along the small stomach curve as a connection between the esophagus & intestine
Thus, the stomach loses a large proportion of its filling volume & only small portions can be taken.
In addition, the hunger hormone ghrelin is influenced, which has a positive effect on the feeling of hunger.
Ghrelin is mainly produced in the parietal cells in the epithelium of the stomach fundus, but also by the ε cells of the abdomen-salivary gland, as well as converted to the active form in a preliminary stage in the hypothalamus and pituitary gland and by cleavage of some amino acids.
Ghrelin is a hormone that regulates food intake and the secretion of growth hormone.
In periods of hunger, the level of ghrelin in the blood rises, after eating it decreases.
Lack of sleep induces increased ghrelin secretion and in this way probably contributes to the development of Obesity.
Other hormones that control the feeling of hunger or satiety are leptin, orexin & cortisol.
In the fasting state, the ghrelin secretion is increased, after eating, the ghrelin level decreases.
From the frequency of the procedure, the gastric reduction, meanwhile, is significantly ahead of the gastric bypass. An advantage over gastric bypass surgery is that no intestinal diversion is required and therefore this procedure is more suitable, for example, for patients with a chronic inflammatory bowel disease Crohn's disease or intestinal adhesions. Further, the absorption of drugs is undisturbed.
But the disadvantage is the irreversible loss of a large part of the stomach.
After a bariatric surgery, the affected person must switch to a special, balanced diet.
Due to the weight reduction, a significant improvement in the general state of health can occur, since many secondary diseases are also favorably influenced.
The tube magenop, is a purely restrictive procedure in which a large part of the stomach is removed.
This means that food can now be taken only in small portions.
About 30% of patients lose 60% of their excess weight after gastric sleeve surgery, as well as a substantial elimination of their concomitant diseases. About 10% of patients do not achieve this reduction in their weight, but lose so much weight that they are satisfied with the result, since most of the concomitant diseases have been eliminated or significantly improved. The rest experience only a minimal weight reduction and are not satisfied with the result.
The cause of insufficient weight reduction are:
No change in eating habits, insufficient physical activity and continued behavioral errors regarding food intake.
Rarely there are anatomical reasons for the lack of weight loss. In some cases, too little was removed from the stomach during the operation. In most cases, however, patients have taken too large amounts of food per serving in the long run and thus gradually caused an increasing dilation of the tubular stomach (dilatation). The gastric tube is a muscle that wears out with constant overstretching, thereby getting bigger again and also allowing larger portions.
Cicatricial narrowing in the gastric tube (stenosis), as a rule, leads to more frequent vomiting and heartburn. This condition, if it occurs early, can possibly be treated with an expansion. This is done without surgery with the gastric mirror over which a balloon is inserted for dilation. Another possibility, in the case of a narrowing that occurred at an early stage, is to insert a self-expanding stent (a tube widening the narrowing). This also happens with the level of the stomach. The stent is removed again after 4-6 weeks. If these measures do not bring about a permanent improvement, an operative correction must be made. The tubular stomach is then preferably converted into a bypass.
Many patients suffer from heartburn even before the operation. Heartburn is provoked by gastric juice flowing back into the esophagus. In many patients, these complaints improve when the body weight decreases. However, in some patients there is no improvement or even an increase in heartburn. In about 8% of patients who did not have heartburn before gastric sleeve surgery, these complaints are newly formed. For the most part, it is possible to improve or eliminate heartburn with acid-blocking drugs. However, when gastric juice, especially when lying down, passes through the esophagus to the larynx, coughing attacks occur, which can be very excruciating and cannot be eliminated by tablets. In this case, only a corrective operation remains, which, as a rule, also consists in the transformation of the tubular stomach into a bypass.
With insufficient weight loss and a greatly expanded tubular stomach, the re-reduction of the tubular stomach rarely leads to good results. This measure should then be combined with an additional bypass operation. That is, the tubular stomach is reduced in size, and in addition, in front of or behind the exit from the stomach, a partial shutdown of the small intestine is made.
Laparoscopic surgery
This is done by keyhole technology, i.e. laparoscopically or minimally invasively, over five small holes in a size of 1.5 to 2.5 cm. The abdomen is first filled with a gas so that the surgeon has a better view of the abdominal interior. Now, the surgeons use a special technique to loosen the stomach from adhesions, for example to the spleen, in order to subsequently perform the actual reduction.
An important sub-step of the operation is the so-called leak test:
at the end of the procedure, the doctor briefly fills the new stomach with a blue liquid via a small gastric tube to ensure that the sutures are absolutely tight.
Thus, the rate of complications in the hands of experienced surgeons is very low.
Wound drainage
Wound drainage is a drainage system for body fluids (drainage), which is usually used after major surgical procedures to temporarily drain blood & wound secretion to the outside or to promote the initial wound healing. The most common wound drainage is redondrainage (named after the Parisian maxillofacial surgeon Henry Redon). At the end of major operations, a wound drainage is inserted into the wound by the surgeon in front of the skin suture in the subcutaneous fatty tissue (subcutis) and guided out of the skin a few centimeters from the wound.
The drainage hose is connected to a container under negative pressure, which allows a continuous suction.
The suction on the drainage causes wound secretion (blood and serous fluid) to be discharged to the outside and the wound surfaces to be contracted. This should bring about a better healing of the wound surface.
A postoperative wound drainage (redondrainage) is usually left for 2-3 days.
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
SILS, Single Incision Laparoscopic Surgery, Antalya, Turkey, price, cost

SILS stands for Single Incision Laparoscopic Surgery.
In contrast to the "traditional" laparoscopic surgery, in which as a rule 3-5 short-distance (10mm) skin incisions distributed over the abdomen are chosen as access, with the SILS technique only an incision of 15-20 mm is made.
This skin incision in the depth of the navel leads to the end the procedure leads to an invisible or barely visible scar, which disappears in the navel.
The navel not only represents the geographical center of man, but also provides the easiest and most safe access to the abdominal cavity. After the skin incision, the actual abdominal wall is displayed and three small working sleeves are inserted through the abdominal wall into the abdominal cavity. In addition to optics with a camera, two more sleeves for instruments are inserted into the abdominal cavity.
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
Mini Gastric Bypass, Antalya, Turkey, Obesity Center, Antalya, Turkey

The Mini Gastric Bypass operation is performed in Antalya, Turkey, laparoscopically.
With gastric bypass, the stomach is separated a few centimeters below the entrance to the stomach. There remains a small residual stomach, "pouch", which holds about 15 ml and serves as a brake for the supplied food. The small intestine is also cut. One end of the intestine is connected to the small residual stomach and the other is diverted in such a way that the food and digestive juices are mixed only in the middle small intestine and the upper small intestine, directly adjacent to the stomach, is bypassed ("engl. Bypass"). The digestive juices are introduced into the deeper parts of the intestine and thus digestion can only begin here by splitting the food components. The consequence is that not all food components can be broken down and thus only a part is absorbed "absorbed". Thus, there are fewer nutritional building blocks available to the blood. The undigested food is transported to the large intestine.
The disadvantages of gastric bypass
The physiology in the digestive process is changed. Not only the intake of calorie carriers is reduced, but also that of vitamins, minerals and trace elements.
In particular, vitamin B 12 can no longer be "absorbed" via the normal digestive performance and the administration must be carried out throughout life by injection.
In individual cases, this also applies to the absorption of iron.
Permanent intake of a multivitamin preparation is required daily.
Certain medications may no longer be taken orally because they can damage the intestinal mucosa.
Others are reduced in their effectiveness, e.g. hormones.
Depending on the food composition, side effects such as flatulence, foul-smelling fatty stools, diarrhea and the so-called "dumping syndrome" with circulatory drop and lightning-like bowel emptying after eating very sugary foods and drinks can occur.
The restrictive effect of the small "pouch" can be lost over time and normal to large amounts of food can then be eaten again.
The execution of an endoscopic gastroscopy is no longer possible, or the removal of bile duct stones.
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
Revision surgeries at the Obesity Center, Antalya, Turkey
Gastric banding for gastric reduction or gastric bypass
Gastric sleeve to gastric bypass, obesity clinic
Gastric Bypass Revision Surgery, Obesity Center, Antalya, Turkey
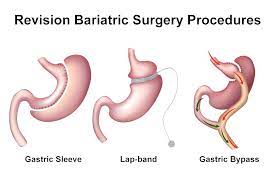
The revision surgeries are performed by the English-speaking doctor, in Antalya, laparoscopically.
Information on corrective surgery after a bariatric procedure
If you have already received an operation for weight loss, it may be that months or years after the operation there will be certain difficulties. This is quite rare and should be discussed in practice. At this point, we would like to provide you with some information in advance so that you can describe and discuss your problems in more detail for a medical consultation.
The following problem groups can be identified, regardless of which intervention was previously performed on you:
insufficient weight loss significant re-increase in body weight despite previous good weight loss.
Complaints caused by frequent vomiting very frequent heartburn, rising of gastric juice with coughing attacks, especially when lying down constrictions in the upper digestive tract with obstruction of passage Ulcer formation in the small stomach pouch Lack of weight loss or a significant increase in body weight after surgery are actually never caused by changes to the operated stomach. Most of the reasons are non-compliance with dietary recommendations, insufficient physical activity (swimming, walking the dog, climbing two stairs a day is not enough). Often, behavioral patterns that have led to overweight and obesity are maintained despite intensive counseling or resumed in frustration situations. These conditions require a new extensive clarification and usually also psychotherapy in order to work up and eliminate the wrong development.
Very rarely, anatomical reasons on the operated stomach or small intestine are the cause for the above-mentioned weight curves. For example, a defective gastric band can lead to an increase in weight, a fistula between the small stomach pouch and the stomach turned off, or a distended tube stomach over time.
In order to find out such causes, an X-ray examination and a gastroscopy are usually required in advance.
Typical complications of the individual surgical procedures will be presented below:
Gastric banding:
a maximum constricted gastric band leads to frequent vomiting several times a day. As a result, the stomach located below the gastric band can turn upwards through the gastric band and thus lead to a passage obstruction. This condition is called slippage. Complete emptying of the gastric band immediately eliminates discomfort. However, as a rule, slippage cannot be eliminated without surgery.
A highly constricted gastric band also leads to an expansion of the esophagus and often to a long-term retention of portions of food in the esophagus with corresponding inflammatory reactions. It can cause reflux of gastric juice and food residues into the trachea while lying down. As a result, coughing attacks occur.
In rare cases, the gastric band can also migrate through the stomach wall and then lie in the stomach, causing weight gain again (arrosion).
All these states require correction. This consists of removal of the gastric band. The removal of the gastric band alone leads to a re-increase in body weight in 99%. Therefore, it is worth considering combining the removal of the gastric band with another procedure (bypass, tubular stomach).
From large statistics it is known that the re-insertion of a gastric band does not have good results.
Tube stomachs:
About 30% of patients lose 60% of their excess weight after gastric sleeve surgery, as well as a substantial elimination of their concomitant diseases. About 10% of patients do not achieve this reduction in their weight, but lose so much weight that they are satisfied with the result, since most of the concomitant diseases have been eliminated or significantly improved. The rest experience only a minimal weight reduction and are not satisfied with the result.
The cause of insufficient weight reduction are:
No change in eating habits, insufficient physical activity and continued behavioral errors regarding food intake.
Rarely there are anatomical reasons for the lack of weight loss. In some cases, too little was removed from the stomach during the operation. In most cases, however, patients have taken too large amounts of food per serving in the long run and thus gradually caused an increasing dilation of the tubular stomach (dilatation). The gastric tube is a muscle that wears out with constant overstretching, thereby getting bigger again and also allowing larger portions.
Cicatricial narrowing in the gastric tube (stenosis), as a rule, leads to more frequent vomiting and heartburn. This condition, if it occurs early, can possibly be treated with an expansion. This is done without surgery with the gastric mirror over which a balloon is inserted for dilation. Another possibility, in the case of a narrowing that occurred at an early stage, is to insert a self-expanding stent (a tube widening the narrowing). This also happens with the level of the stomach. The stent is removed again after 4-6 weeks. If these measures do not bring about a permanent improvement, an operative correction must be made. The tubular stomach is then preferably converted into a bypass.
Many patients suffer from heartburn even before the operation. Heartburn is provoked by gastric juice flowing back into the esophagus. In many patients, these complaints improve when the body weight decreases. However, in some patients there is no improvement or even an increase in heartburn. In about 8% of patients who did not have heartburn before gastric sleeve surgery, these complaints are newly formed. For the most part, it is possible to improve or eliminate heartburn with acid-blocking drugs. However, when gastric juice, especially when lying down, passes through the esophagus to the larynx, coughing attacks occur, which can be very excruciating and cannot be eliminated by tablets. In this case, only a corrective operation remains, which, as a rule, also consists in the transformation of the tubular stomach into a bypass.
With insufficient weight loss and a greatly expanded tubular stomach, the re-reduction of the tubular stomach rarely leads to good results. This measure should then be combined with an additional bypass operation. That is, the tubular stomach is reduced in size, and in addition, in front of or behind the exit from the stomach, a partial shutdown of the small intestine is made.
Gastric bypass:
For gastric bypass with regard to insufficient weight loss or renewed weight gain, the same explanations apply as just indicated for the tubular stomach. The small portion of the stomach (stomach bag, technical term: stomach pouch) can also expand in case of too large food portions and absorb more food again. However, it is more important that the connection between the stomach pouch and the subsequent small intestine also widens and thus the food can slip out of the pouch into the small intestine much faster. This condition is basically due to an undisciplined eating behavior. A correction in the sense that the pouch and the connection between the pouch and the small intestine are reduced rarely leads to good results, the weight loss is low and does not last long. Studies are currently underway to determine whether an additional constriction of the stomach pouch with a plastic ring results in an improvement. However, as a rule, a new nutritional consultation and also psychotherapy is required to treat the continuing disorder in food intake.
Constrictions (stenosis) between the stomach pouch and the subsequent small intestine are rather rare, usually occur a few weeks after the operation and can usually always be eliminated with a balloon dilation with the help of the gastric level.
In about 7% of patients with gastric bypass, ulceration occurs at the transition from the gastric pouch to the small intestine. These ulcers are observed almost exclusively in heavy smokers or in patients who continue to take painkillers from the group of rheumatic drugs. The ulcers can usually be healed with medication. However, it is important that the patient quits smoking and switches the painkillers to stomach-friendly drugs. In extremely rare cases (bleeding, stomach wall breakthrough), surgery is indicated for correction.
Summary:
Each operation has its specific risk. The initial interventions for weight loss show a pleasantly low complication rate despite the usually significant concomitant diseases. This does not apply to repeated interventions. Even with reduced weight, the complication rates are significantly higher. If complications occur between 5-7% during the first intervention, the complication rate for the first corrective intervention is 15-25%, for further corrective operations the risk of complications increases to 50%. The correction of an existing method (i.e. correction of a gastric bypass) does not have good results, as a rule, one should switch to another method. In our own experience, we then see patients who benefit very well from the new procedure. But there are also patients who, despite the changed surgical procedure, are only slightly successful
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
Type 2 Diabetes Surgery in Turkey, Antalya (English speaking doctor)
Gastric sleeve or mini gastric bypass, Obesity Center, Antalya, Turkey

The diabetes operation is performed by a english speaking doctor,
in Antalya, performed laparoscopically.
Gastric surgery lowers blood sugar levels.
If conventional weight reduction is not possible, gastric surgery can help with type 2 diabetes.
With the gastric reduction or gastric bypass at the obesity Center in Antalya, Turkey, it is possible in most cases to significantly reduce blood sugar levels. Many patients no longer need to inject insulin after surgery. The risk of dangerous diabetes complications such as heart attack, stroke, eye, vascular & kidney diseases decreases.
There are several methods:
1.) Stomach reduction (gastric sleeve), the success rate here is 80%.
2.) The best results were obtained after a mini gastric bypass.
Here, switching off the stomach is carried out, bypassing the duodenum.
The operation is performed laparoscopically, that is, by means of "keyhole surgery".
Immediately after the operation, there should be a decrease in the required insulin therapy.
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
Heartburn Treatment / Reflux Surgery, Antalya,Turkey
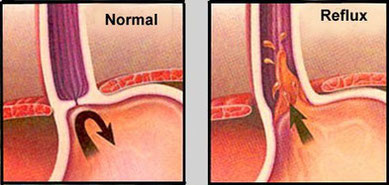
The heartburn treatment / reflux surgery is performed by english-speaking doctor, in Antalya, laparoscopic performed.
Heartburn treatment / reflux surgery is mainly used for extremely severe heartburn, which has been plaguing the affected person for a long time and does not respond to any treatment methods.
It can not only relieve the patient of his complaints, but also put an end to the associated psychological stress.
Everyday life then often seems like an insurmountable obstacle and the mental state is often impaired. A reflux surgery can give these sufferers a piece of quality of life.
What happens during reflux surgery?
The primary goal of reflux surgery is to prevent the path of stomach acid from the stomach into the esophagus. This effort is directed not only against the acute symptoms that an untreatable reflux brings with it, but above all against its long-term consequences.
So that exactly this does not happen, doctors have developed antirefluxplasty, i.e. surgical techniques against occurring reflux. This ensures that ingested food can pass through the esophagus as usual, in order to then be crushed and utilized in the digestive tract. The chyme fills the upper part of the stomach, but this area expands and thus narrows the transition from the esophagus to the stomach. The effect: A backflow of the stomach contents is hardly possible anymore.
Most patients no longer or hardly suffer from annoying heartburn afterwards.
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
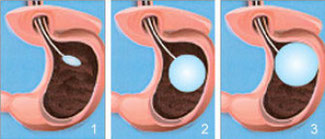
Gastric balloon filled with air or liquid, Antalya, Turkey
english speaking doctor, Obesity Center Antalya, Turkey
Gastric balloon filled with air or liquid, Antalya, Turkey
By using a gastric balloon in conjunction with a
under the supervision of a dietary change, serious health disorders of obesity patients can be significantly reduced and at the same time a new quality of life can be achieved.
The gastric balloon system consists of a soft, stretchable balloon, an insert tube & a filling system.
The balloon can be inserted and removed through the mouth - without surgery or cuts.
If the empty balloon is in the stomach, it is filled with a sterile saline solution.
The filling quantity is individually adapted to the patient and varies between 400 - 700 ml.
The balloon of the system now floats freely in the stomach and partially fills it.
The patient already achieves a feeling of satiety with a much smaller amount of food & from now on takes less food.
Air-filled or liquid-filled gastric balloon?
The gastric balloon can be filled with either liquid or air. Some doctors are critical of the air-filled variant for several reasons: on the one hand, a leak in the air-filled gastric balloon is not noticeable so quickly, since the blue coloration of the urine is absent. This also increases the risk of the balloon entering the intestine and thus of intestinal obstruction. It is also possible that the weight reduction of the air-filled balloon is worse, since it weighs only about 30 grams. The liquid-filled gastric balloon, on the other hand, has a net weight of about 450 to 700 grams and thus ensures a faster feeling of satiety.
The disadvantages of the gastric balloon:
The gastric balloon may burst.
The gastric balloon makes the stomach bigger and you can absorb even more food after removing the balloon.
If you want to have a stomach reduction after the gastric balloon,
this is a revision operation and costs accordingly more.
Especially in the first days after the onset, the side effects of a gastric balloon can be significant. Typical are nausea, abdominal cramps and a pronounced feeling of fullness. These complaints settle as soon as the stomach gets used to the foreign body. This is usually the case after about three to seven days. However, even in the long term, some patients complain of a constant feeling of pressure or fullness, belching and heartburn. If the gastric balloon causes permanent problems, it should be removed ahead of time.
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
Elipse gastric balloon for swallowing, Antalya, Turkey

The gastric balloon for swallowing allurion Antalya, Turkey
The swallowable gastric balloon Elipse ™ from the company Allurion is an innovative treatment method for weight reduction, which has already become established worldwide.
Conventional gastric balloons are inserted endoscopically into the patient's stomach via a tube by gastroscopy. The company Allurion has developed a novel variant of gastric balloon treatment: the swallowing balloon Elipse ™ . The great advantage of this development is that comfortable weight reduction is possible without surgery, without endoscopy and without anesthesia as part of the Elipse ™ balloon program.
Elipse ™ Gastric Balloon Treatment: How it Works
The Elipse ™ gastric balloon is placed in the patient's stomach and reduces its volume. As a result, patients can no longer eat so much and get full faster. The gastric balloon can thus support people in losing weight who have not been successful with other methods so far and help them to a healthier life.
The special feature of the Elipse ™ gastric balloon is the type of treatment, i.e. the insertion and removal of the balloon. The Elipse ™ gastric balloon is a so-called swallow balloon. It is emptied by the patient, swallowed down in the form of a capsule and as soon as it has arrived in the stomach, it is filled with a liquid via a fine tube attached to the capsule. Subsequently, the tube is carefully withdrawn by the doctor, and the patient can go home.
Removal of the Elipse ™ gastric balloon
The Elipse ™ gastric balloon empties all by itself via a timed release valve that opens after about 16 weeks. The soft shell of the balloon is excreted naturally through the intestine, without the need for any intervention.
Anaesthesia: no anaesthesia necessary, non-surgical procedure
Duration: Treatment lasts about 20 minutes, outpatient
Scope: 4 months of wear
Sociability: Immediately socially acceptable again, if necessary 2-3 days
Do the health insurance companies participate in the Elipse ™ gastric balloon treatment?
No, the health insurance companies do not participate in the Elipse ™ gastric balloon treatment.
The costs for the Elipse ™ program must be borne by the patient himself.
What side effects can occur?
The gastric balloon makes the stomach bigger and you can absorb even more food after removing the balloon.
If you want to have a stomach reduction after the gastric balloon,
this is a revision operation and costs accordingly more.
Especially in the first days after the onset, the side effects of a gastric balloon can be significant. Typical are nausea, abdominal cramps and a pronounced feeling of fullness. These complaints settle as soon as the stomach gets used to the foreign body. This is usually the case after about three to seven days. However, even in the long term, some patients complain of a constant feeling of pressure or fullness, belching and heartburn. If the gastric balloon causes permanent problems, it should be removed ahead of time.
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
Gastric Sleev Plication, (laparoscopic) only in Antalya, Obesity Center
The POSE2 Endo-Sleeve, Pose procedure, Apollo procedure, Gastric Sleeve Plication, or also known as gastric Sleeve, is a novel laparoscopic treatment for stomach reduction.
In Turkey, this procedure is performed laparoscopically.
A large part of the stomach is folded and sutured from the outside.
Thus, the stomach loses a large proportion of its filling volume & only small portions can be taken.
The stomach volume can be reduced by up to 75%.
In Germany, the stomach volume is reduced by about 25%.
The disadvantages of stomach folding:
If you have a tumor in the stomach, unfortunately you can not see it if it is in the folded area.
You will always be hungry, since the hunger center is not removed, as with the tube stomach, Gastric sleeve,
or in the case of stomach reduction.
This operation cannot be reversed.
If food or drinks get into the clamped stomach, they can not drain into the intestine.
(if it is performed endoscopically as in Germany)
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
Botox injection into the stomach, Antalya, Turkey (endoscopic)

How does the anti-hunger syringe help?
How much excess weight can you lose with gastric botox treatment? The treatment is carried out as part of a day–by–day endoscopic treatment - gastroscopy - at very specific points in the stomach. The patient receives sedation beforehand and thus does not feel any pain. As a result of the treatment, the emptying of the stomach is delayed, and the feeling of hunger is reduced. This gradually leads to weight loss. Controlled double-blind studies show that by using the "anti-hunger syringe" a weight loss of 5 to 15 kilograms is possible within six months. After that, if necessary, a repetition of treatment is possible.
The attending physician should be specially trained in the latest gastric botox technique. Because the desired effect, i.e. weight loss, can only be achieved by applying it in the right places.
Do you have any questions?
Handy: +90 531 421 40 02
Here you will find the doctors team:
Here you can find the Turkish holidays:
Here you can find food after surgery:
Here you will find films about the stomach operations:
Here you will find the prices for all operations in Turkey:
Here you will find before / after pictures of the patients Part 1
Here you will find before / after pictures of the patients Part 2
Here you will find before / after pictures of the patients Part 3
Here you will find before / after pictures of the patients Part 4
Here you will find before / after pictures of the patients Part 5
Here you will find before / after pictures of the patients Part 6
Contact form:
All the surgeries / treatments we offer at the Obesity Center in Antalya, Turkey
Stomach Reduction Antalya Turkey
Sleeve Gastrectomy Antalya Turkey
Gastric Sleeve Resection Antalya
SILS, Single Incision Laparoscopic Surgery
Mini Gastric Bypass Antalya Turkey
Bipartition Bypass Antalya Turkey
Duodenal Switch Bypass Antalya
Omega loop Bypass Antalya Turkey
Roux En Y Bypass Antalya Turkey
Revision operation: Gastric band to Gastric Sleeve Antalya Turkey
Revision operation: Gastric Sleeve to Gastric Bypass Antalya Turkey
Revision operation: Gastric Bypass Antalya Turkey
Type 2 Diabetes Surgery Antalya
Heartburn Treatment / Reflux Treatment Antalya Turkey
Gastric Sleev Plication, Antalya Turkey
Gastric balloon filled with liquid Antalya Turkey
Gastric balloon filled with air Antalya Turkey
Elipse gastric balloon for swallowing, Antalya, Turkey










